In honor of Earth Day, this is the second annual Blog Post Recycling Day. I think it is the second annual Blog Post Recycling Day. Somebody declared one last year, and I recycled then, but I haven't actually seen anything about it this year. Maybe because my Facebook friend who posts that kind of stuff is in church today?
Anyway, it's timely -- just one week from Johnson County, Iowa's NAMI Walk. So my recycled blog from a month ago comes with one more plea to contribute to the organization that has contributed so much to me, making my contribution to you, dear readers, possible.
Please, please, please, click on the button to
To find out why, read:
Friday, March 25, 2011
On The Road Again -- NAMIWalks 2011
 It's that time of year again. Across the country people with mental illness, our friends, family, care providers, even law enforcement officials are pulling on our walking shoes to raise money for NAMI -- National Alliance on Mental Illness. Last year soldiers in Iraq pulled on their hiking boots and their 40 lb. packs and ran while NAMI San Diego walked.
It's that time of year again. Across the country people with mental illness, our friends, family, care providers, even law enforcement officials are pulling on our walking shoes to raise money for NAMI -- National Alliance on Mental Illness. Last year soldiers in Iraq pulled on their hiking boots and their 40 lb. packs and ran while NAMI San Diego walked.So what is this all about? Here, my friends, is my testimony.
A couple years ago, I wrote a post on holiday gift giving for your favorite normal. I asked my spouse, What would be a good present for the family member of somebody with a mental illness?
She didn't even look up from her computer. Without missing a beat, she said, A cure.
A cure. I know that mental illness is a family illness. The whole family lives with it. But her words caught me. What she wanted was for both of us, a cure.
It's something she can't give me. I can't give her. My doctor can't. You can't give it to the person you love.
We can, however, learn to manage symptoms. We can claim the very best lives we can live. We can live in recovery.
Peer To Peer Program
I learned about recovery from NAMI, from their Peer to Peer program. P2P is a ten-week course taught by people with a mental illness for people with mental illness about what we do after the doctor hands us a diagnosis and a prescription.
P2P teaches us how to live. It is why I bust my butt for this walk. It's not a cure. But it's a lot.
That first class, I heard that I am not alone. The very first note I took said, More unites us (our experiences) than divides us (our diagnoses.)
Next P2P showed me the immense dignity of those who live with mental illness. It made me proud to know and be known by and be in community with others who live with mental illness.
It supplied tools like dialectical thinking, mindfulness, relapse prevention planning, techniques for emotional regulation and getting a good night's sleep, strategies for staying safe and coping with hospitalization.
P2P gave me something to do when medication didn't give me a cure.
And it opened for me a path into my future. It reminded me that I am an advocate. That is who I am. I still have an identity, after all
So I bust my butt for this walk. It is how I give back.
NAMI Walks
Now, the first time I did a NAMI walk, to tell the truth, I was scared. Would it be grim? A protest and a wailing against what is not possible, what we have lost and what we have to face?
If you have walked for NAMI, you are laughing here. You know a NAMI Walk is so -- not grim. It's a party! With balloons and babies and dogs, music, belly dancers, football players, great food. In Johnson County, Iowa, the Old Capitol City Roller Girls lead off the walk. In San Diego, you are likely to hear a didgeridoo.
Bottom line, a NAMI walk is a gift. It's a public demonstration to our families, friends, politicians, our neighbors, coworkers, the people in our places of worship, the viewing public -- a public demonstration that we are here for each other. We take a break from all that wailing. And throw a whale of a party.
At the same time, we raise funds for the programs that help us help ourselves and one another, the things that nobody else will pay for, for people who have fallen off the bottom of the budget. NAMI does the stuff that makes a difference the day after the doctor hands us a diagnosis and a prescription.
Team Prozac Monologues debuted last year, with results that were not too shabby. We raised $2640. Mazie's sponsors contributed $250 toward that total. Helen is walking in her stead this year. Sponsors can contribute in Mazie's memory here.
Why I Walk
Me, I am walking for everybody who used to be on a three month wait list for an intake interiew at the local community mental health center; but this year that became a six month wait list at the center the next county over. I am walking for everybody who used to be on a four year wait list for sheltered housing; but this year the shelter shut down.
I am walking for those who are not crazy enough to pull out a gun and get the sheriff to buy their meds; they're just crazy enough to sleep in the alley behind the homeless shelter after they have stayed their ninety-day limit.
I am walking for family members who go to work wondering what is happening at home with their loved ones, now that the day program is closed.
I am walking for the resident on call in the ER who has to send home the merely suicidal, while the flaming psychotic waits for 36 hours in the hallway for the next available bed. And for the newly diagnosed and dazed person who just got released with not enough meds to make it through the weekend, to make room for the flaming psychotic.
I am walking for the young people I know whose brains are even now being damaged in a war that we got into for oil.
I am walking in gratitude for law enforcement personnel who are trying to figure out how to do this new job, and need new training, to take care of those who have been discarded so that the very richest people in the world can get a tax cut. I am walking in prayer for those who get caught up in somebody's suicide by cop.
This would be the place to note that the co-chairs of Johnson County's NAMI Walk this year are Janet Lyness, County Attorney, and Lonnie Pulkrabek, County Sheriff. Props to them and to the competition between their two teams!
I did say that the Walk would be a party. So even while I am angry that so much suffering comes not from the illness, but from the neglect, I will nevertheless celebrate those who do what they can do. (That sentence would be an example of dialectical thinking, by the way -- see above, the curriculum of Peer to Peer.)
I am walking in wonder and amazement at the strength of the human spirit. I am walking in deep appreciation for those who have helped me personally, for peer teachers, support group members, care providers, friends and family.
I will be walking with tears in my eyes, that my son and daughter-in-law will travel from Madison to Iowa City to walk beside me.
I am walking on April 30, 2011 in Iowa City, Iowa for all these reasons. And I am walking also for you, dear reader. I ask you to support me in this walk. Click here to make your tax deductible, safe and quick contribution to NAMIWalks Johnson County.
Closing Shot
There are many versions of this song on Youtube. I chose this one, despite the credits that run over it, because the ragged bunch of friends who sing it, some not sure of the words, illustrate the point. We are a ragged bunch. And pretty wonderful because of it.
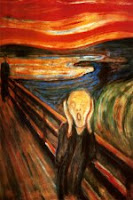
The Scream by Edvard Munch in public domain
photo of Team Prozac Monologues by Judy Brickhaus
photo of homeless vet by Matthew Woitunski and used under the Creative Commons licencse
photo of New York City police officer by See-ming Lee, copyrighted and used by permission
photo of Team Prozac Monologues by Judy Brickhaus
photo of homeless vet by Matthew Woitunski and used under the Creative Commons licencse
photo of New York City police officer by See-ming Lee, copyrighted and used by permission